Before there was technology to assess thyroid hormones in labs, there was this marker…
Cholesterol!
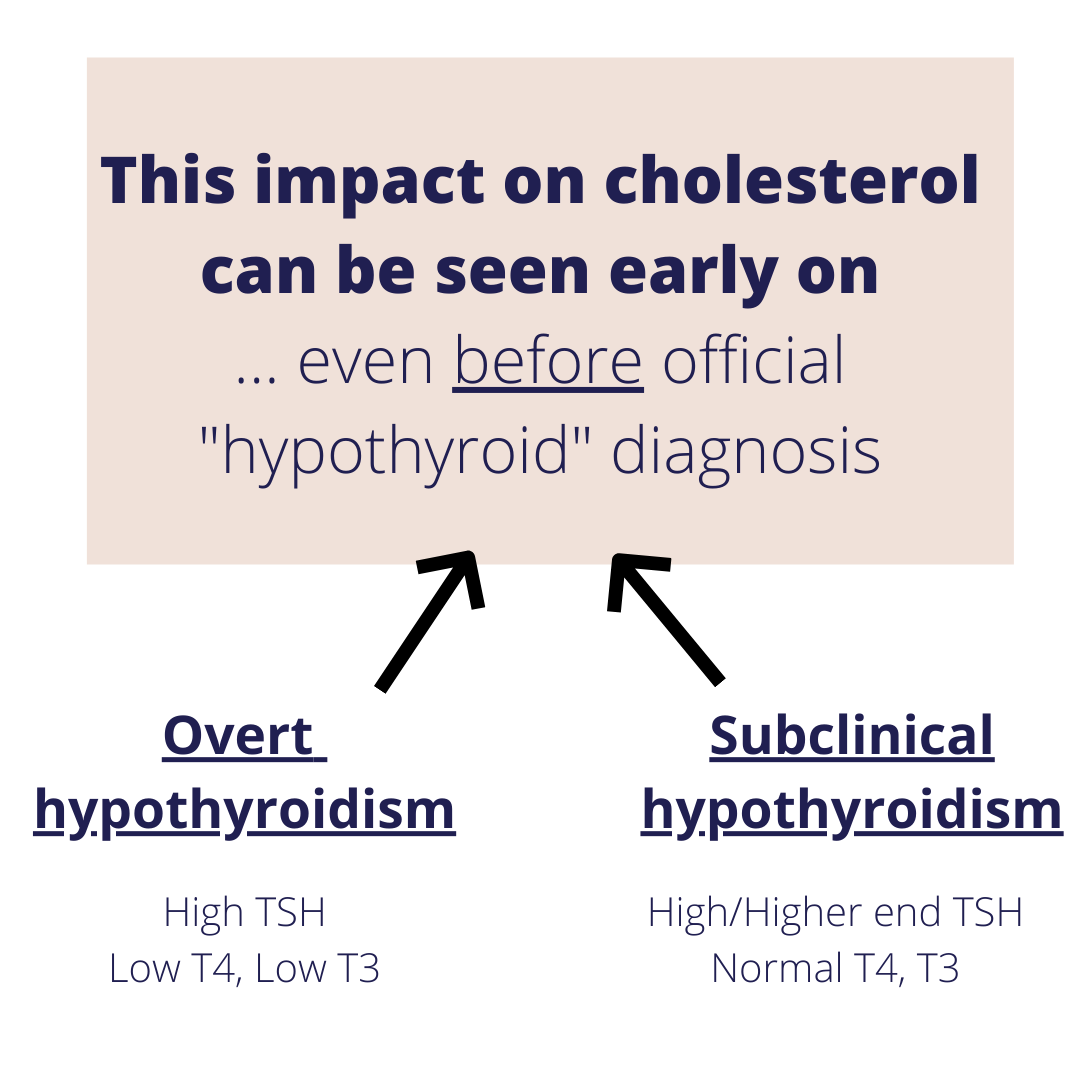
Almost a century ago, medical scientists in the 1930’s discovered that suboptimal levels of thyroid hormone led to compensatory increases in cholesterol. Further, they found that thyroid hormone replacement nearly always improved cholesterol status in those with hypothyroidism. Since this revelation, it has been widely accepted that one of the earliest signs of hypothyroidism is an increase in cholesterol. However, over the past nearly 100 years, the significance of this association has been slightly lost. With a plethora of cholesterol lowering medications as well as an increasing prevalence of other major contributors to elevated cholesterol (inflammation, blood sugar dysregulation, etc.), hypothyroidism (both overt and subclinical) as a root cause has become more taboo.
Before we discuss the connection between thyroid and cholesterol, let’s briefly review cholesterol, what it does, and how it’s made. Understanding this will help to appreciate how thyroid levels impact this especially important part of our body— cholesterol!
What is cholesterol?
Cholesterol is a waxy substance your body needs it to build cells, make vitamins, and produce hormones. A cholesterol is a sterol, a type of lipid (fat). Cholesterol is biosynthesized by all animal cells and is an essential structural component of animal cell membranes. Read: cholesterol is an essential part of being a human being. It is so important that our bodies are actually capable of making it— that’s what “biosynthesize” means. We get dietary cholesterol from animal products, but when measuring cholesterol in your blood during a fasted state, those cholesterol numbers reflect the endogenous (or internal) natural production.
Cholesterol is used to make hormones including sex hormones (estrogen, testosterone, progesterone), stress hormones (cortisol), as well as vitamins including Vitamin D. It is incorporated into every single cell in the human body and helps to add to the integrity of the cell membrane (the fortress around your cells). Additionally, cholesterol is used to make bile, which is an integral part of digestion. Bile also exhibits anti-microbial effects to help keep harmful pathogens outside of your intestinal tract.
Cholesterol is synthesized (created) in the liver in a process catalyzed by an enzyme called HMG-CoA. This is a rate limiting step in cholesterol production— meaning that cholesterol production is directly impacted by this particular reaction. (Remember this because thyroid has a big impact here). Cholesterol is then transported from the liver and into circulation via lipoproteins.You will likely recognize lipoproteins by their more colloquial names like LDL (low density lipoprotein) or HDL (high density lipoprotein). Lipoproteins are classified by their size and density. Some lipoproteins, like LDL, take a larger role in bringing cholesterol into circulation while HDL bring it back to the liver for recycling. This idea is what provides the classification of “bad” versus “good” cholesterol, respectively. Cholesterol, however, isn’t inherently bad– rather it’s the lipoproteins being referenced. This is a common misconception as the good/bad is more specific to the type of lipoprotein and not actual cholesterol.
Cholesterol elevations are oftentimes a symptom of an underlying imbalance somewhere. I tell my clients to think of cholesterol like a firefighter. If a house burns down, the firefighter shows up to put out the flames. Just because the firefighter is there, however, does not mean that he/she started the fire. Think of cholesterol in the same light— that cholesterol shows up to help. Unfortunately, cholesterol has been labeled guilty by association for a long time!

Since the cholesterol being evaluated in labs is usually during a fasted state, it is more reflective of internal production. With that, one may be curious what causes it to increase out of genetics. The list includes, but is not limited to:
… and lots more!
So how does the thyroid fit into this picture?

Thyroid hormones are the main regulators of cholesterol levels by playing an integral role in:
Production:
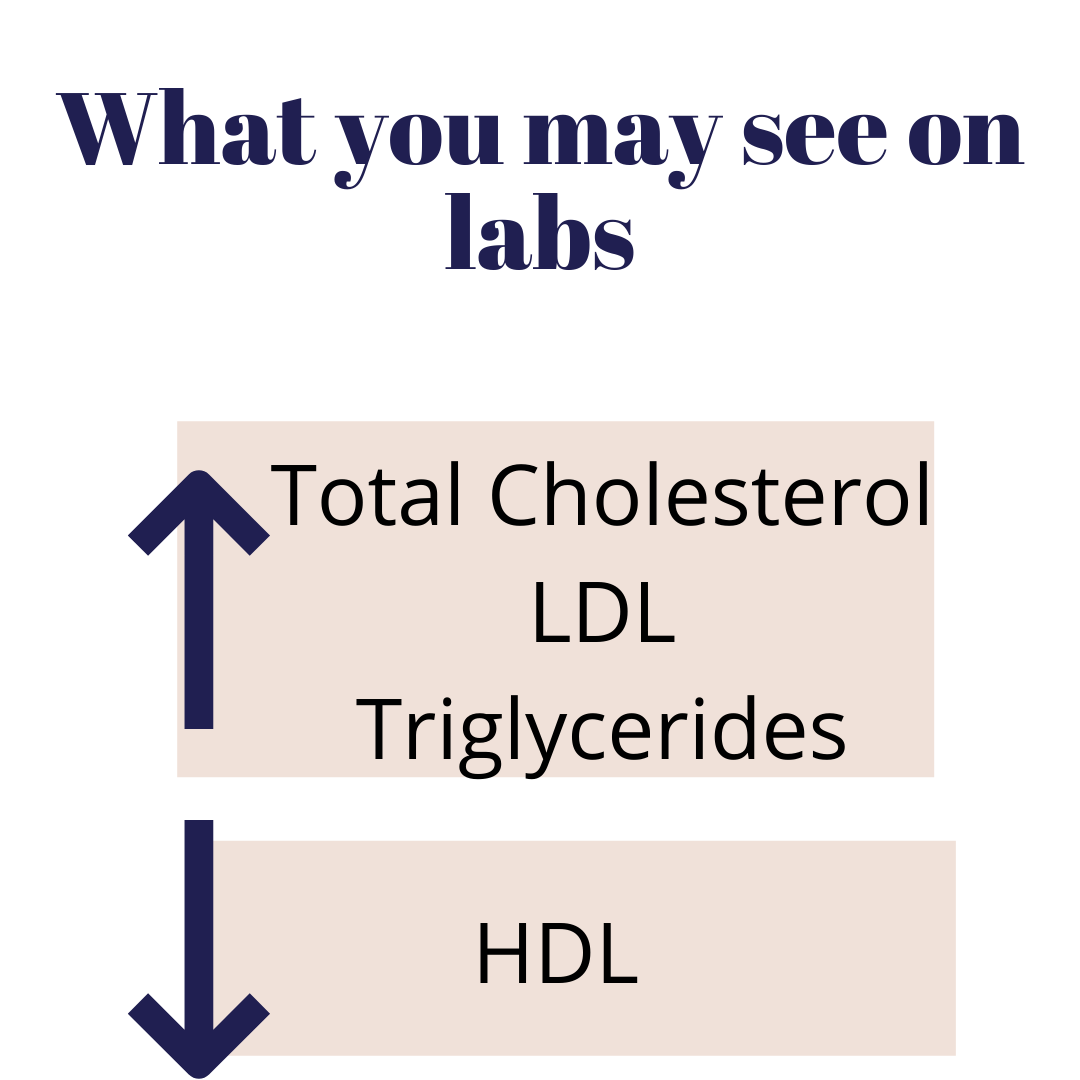
T3 hormone is the main modulator of the HMGCoA enzyme. Depending on whether the body needs more or less cholesterol, T3 steps in to send the signal to HMGCoA to increase or decrease the liver’s synthesis of cholesterol. When T3 levels are low, HMGCoA levels increase, which means that production of cholesterol is also increased. Fun fact: many cholesterol lowering medications act on the HMGCoA enzyme.
Mobilization:
Thyroid hormone also regulates the transport of cholesterol from the liver and into circulation to be taken up by the cells and tissues in the periphery. When thyroid hormones are deficient, cholesterol is not transported adequately and can then build up in the liver. Additionally, low thyroid hormones also decrease the function of the cholesterol receptor sites on cells— meaning that the circulating lipoproteins that carry the cholesterol do not have a place to dock and will then build up in circulation (AKA what you see in your labs).
Reverse transport:
Once the cells are done with cholesterol and/or the liver needs it for another job (like producing bile), lipoproteins like HDL carry cholesterol back home. This is another process where thyroid hormones play a role. Low thyroid hormones decrease circulating levels of HDL which means fewer of the cholesterol carrying lipoproteins are brought back to the liver and therefore are kept in circulation. Additionally, because thyroid hormones play a role in the breakdown and excretion of cholesterol and triglycerides, low thyroid hormone can lead to not enough of these lipids (fats) being degraded.

If you have hypothyroidism AND high cholesterol, what can you do?
Remember this: modern-day diseases, like arterial plaque from high cholesterol, are often brought about by modern-day habits– not by foods that have been around for many millennia. Just a thought! 🙂
Disclaimer: Please note that “Thyroid School” emails from Chews Food Wisely, LLC (and Nicole Fennell, RD) are not intended to create any physician-patient relationship or supplant any in-person medical consultation or examination. Always seek the advice of a trained health professional about any questions you may have regarding a medical condition and before seeking any treatment. Proper medical attention should always be sought for specific ailments. Never disregard professional medical advice or delay in seeking medical treatment due to information obtained in “Thyroid School” emails. Any information received from these emails is not intended to diagnose, treat, or cure. These emails, websites, and social media accounts are for information purposes only. The information in these emails, websites, and social media accounts is not intended to replace proper medical care.
Works cited:
https://doi.org/10.3389/fendo.2018.00511
doi: 10.1056/NEJM193012252032601
10.2174/1874192401105010076

EMAIL:
hello@chewsfoodwisely.com
VIRTUAL APPOINTMENTS ONLY
Business Mailing Address:
2525 Robinhood Street
Houston, Texas 77005
© 2026 Chews Food Wisely. All Rights Reserved. Website Designed by AVM
Disclaimers | Privacy Policy | Terms of Purchase | Terms and Conditions