If I’ve not been clear enough about my stance on carbs, allow me to shout from the virtual rooftops that I am Team Carb… especially for my fellow hypothyroidism pals!
Notice I emphasized that hypothyroid warriors ESPECIALLY need carbohydrates in their diets.
Before I argue my case, let’s break down the science behind carbohydrates and why they’re so dang important.
Carbohydrate: or carbs, are sugar molecules. Along with proteins and fats, carbohydrates are one of three main nutrients found in foods and drinks. Your body breaks down carbohydrates into glucose. Glucose, or blood sugar, is the main source of energy for your body’s cells, tissues, and organs. While it is possible to survive on ketones that are produced with carbohydrate intake is low, this is a survival mechanism and not intended for the long-term. Beyond that, if given the choice, I’m sure most people would rather run off of “preferred” fuel instead of “survival” fuel.
“Carbohydrate” as a food group encompasses quite a few different types of foods including:
Carbohydrates are metabolized and eventually broken down into smaller particles, namely a sugar called glucose. Glucose is the primary and preferred source of fuel for the cells. The cells in the body take up glucose and use it to run all the cellular functions to produce energy. Think of glucose as investing in a new business— it takes money to make money, right? In the body, we must intake glucose to then produce the energy necessary for the body to function.
While we ideally get the majority of glucose from the food we eat, there is a short-term safety net of sorts that kicks into gear when glucose influx from food is limited or glucose levels drop between meals. Stress hormones, including adrenaline and cortisol, kick into gear to send signals to the body to release glucose into circulation from the liver and muscles. Yep, muscles. The body likes to hold onto fat as lonnnnng as possible, so it’s the muscles that get sacrificed.
There are a few metabolic vocabulary words to note:
Okay, so at the end of the day, our body needs glucose. It will obtain glucose from food or from stress hormone release, so what’s the big deal?
I am so glad you asked 😉
It’s all about messaging. What message is your body receiving from how it’s sourcing the glucose it desperately needs?
Scenario One:
Balanced and consistent intake of carbohydrates spread over the day. Paired with protein, fat, and fiber for energy, longevity, and satiation.
Your body: “I am safe. I’m well nourished. I have plenty of fuel to support all of my functions. I think it’s safe right now to maintain my metabolic rate, produce energy, allow for hormone creation, digest this food, and get a good night sleep. Yeah!”
Scenario Two:
Carb restriction. Reliance on stress hormones to get glucose from storage (muscles, liver).
Your body: “NOPE!”
Why is this especially important for hypothyroidism?
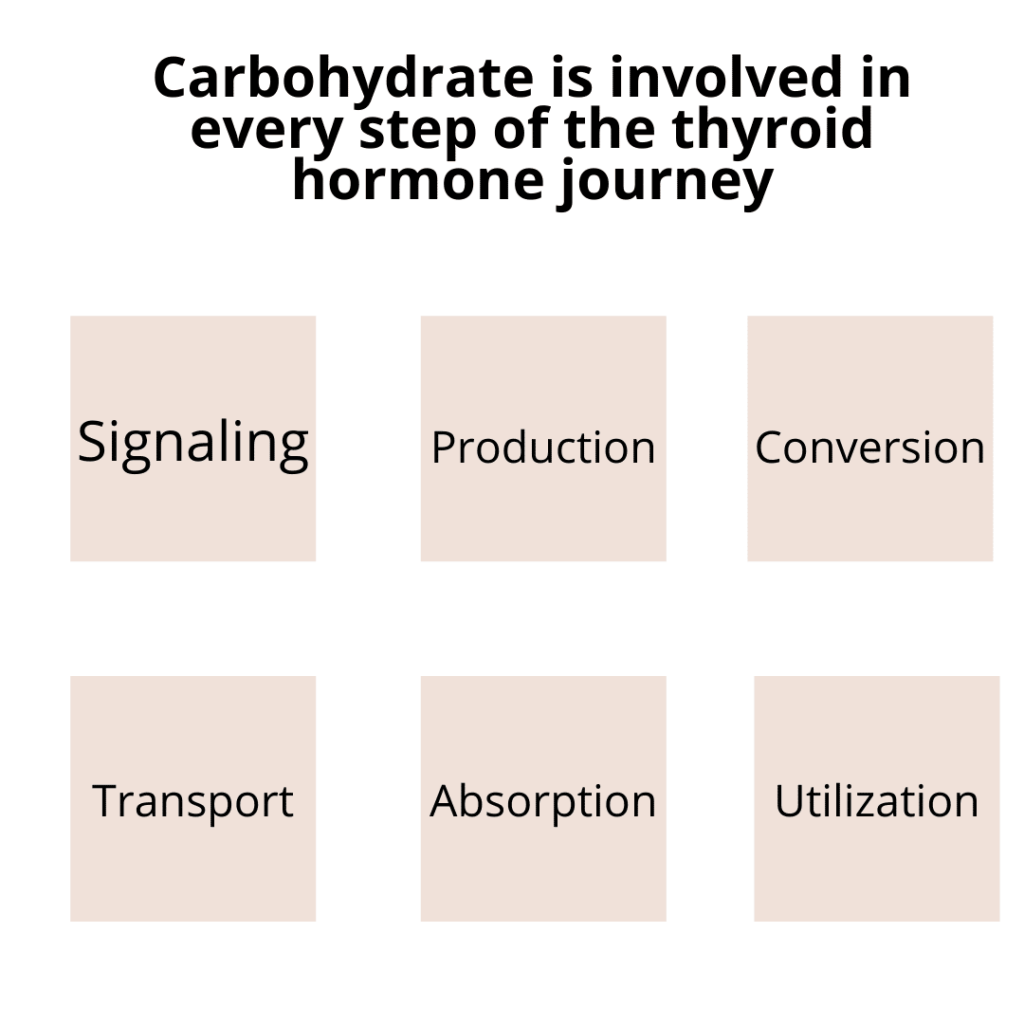
Let me review the journey of thyroid hormone creation and utilization for you…
1. Signaling: Thyroid hormone production begins in the brain with a signal sent from brain to thyroid. Without proper signaling, the thyroid doesn’t get the memo. Cortisol can have two effects on the brain stimulation via the TRH/TSH release: it can either block the secretion as a result of decreased signaling of the hypothalamus and pituitary gland (remember, TSH is a pituitary hormone) from chronic stress. Otherwise, studies show that there are times when TSH is actually elevated in response to high cortisol— indicating true/subclinical hypothyroidism. TSH is also considered a “glycoprotein”— remember that term (reminder: carbohydrate dependent)
2. Production: once the thyroid is signaled to produce more thyroid hormone, it needs building blocks to do so. Building thyroglobulin, or the “blank canvas” for creating T4 and T3 hormones, is a carbohydrate dependent process that is down regulated with inadequate and consistent intake of carbohydrate. In fact, thyroglobulin is a “glycoprotein”– just like TSH. Additionally, the uptake of iodine via the sodium/iodine symporter on thyroid follicles is part of the sodium/glucose co-transport family. Lastly, studies have shown that T3 levels are lower in those following a high fat diet versus a high protein diet— likely related to the body’s affinity for using amino acids for gluconeogensis more than fatty acids.
3. Conversion: once in circulation, T4 accounts for about 80% of what is produced and the remaining is predominantly T3. Since T4 has less bio-activity, it must convert into T3 via deiodination, to be utilized by the cells in the periphery. This conversion requires adequate glucose as it is stimulated by insulin. (Glucose levels prompt insulin secretion). In fact, numerous studies have shown a major down-regulation in the T4 to T3 conversion with starvation. Even in the presence of thyroid hormone replacement, there was an impairment in conversion of T4 to T3 when starvation was mimicked. Lastly, the stress hormone cascade that is released when carbohydrates are restricted actually leads to a preference for T4 converting to Reverse T3— an inactive form of T3. There are animal studies that show that feeding carbohydrates led to significant increase in T3 levels. Contrary, some studies show that a high glucose load decreased this conversion in those with insulin resistance. The takeaway— it’s about balancing carbs… especially for your unique carb tolerance situation. Insider tip: even those with insulin resistance from PCOS or pre-diabetes can and should have some carbohydrate in their diets!
4. Transport: thyroid hormones are transported primarily via Thyroxine Binding Globulin (TBG). This is sort of like the postal service— delivering T4 to target sites where it can be converted and used by the cells in the periphery. As with anything in the body, TBG levels have a sweet spot. Too much TBG can cause low levels of “free” hormone (which is what your cells actually use) and lead to hypothyroid symptoms. When TBG levels are high, the percentage of free thyroid hormones drops. This shows up in labs as low T3 uptake and low free T4/T3. What do carbohydrates have to do with this? You guessed it— it comes back to the stress response. Chronic stress release from inadequate consumption of carbohydrates forces the liver to work overtime to perform glycogenolysis (breakdown of glycogen for fuel) and gluconeogensis (creation of new glucose). The liver does a LOT of things, but when its focus is on energy production, some other things can fall to the wayside, including clearing excess estrogen from the circulation. Excess estrogen can lead to “estrogen dominance” which leads to high levels of TBG, and eventual low levels of free hormone available.
5. Utilization & Absorption: lastly, the little receptors outside of our cells that allow thyroid hormone uptake can become resistance when stress hormone is too high and/or food intake too low. Low carbohydrate intake can lead to too low insulin levels— which is used in many steps along the thyroid hormone journey. I covered this in one of my last posts that under-eating, especially carbohydrates, can worsen cellular resistance. Additionally, the stress hormone effect on cellular sensitivity to thyroid hormones diminishes the higher and longer stress hormones stick around.
Okay, this is a LOT of information, so what do you do with this?
1. Avoid extremes. Our bodies really like balance, predictability, and routine. Before you jump on the low-carb, intermittent fasting, HIIT bandwagon, ask yourself, “What message is my body receiving?”
2. Don’t be afraid of carbohydrates. Ideally, carbohydrate choices would come from mostly whole-food sources like root vegetables, beans, etc. Whole foods are perfectly designed and provide more than just carbs— oftentimes touting vitamins, minerals, proteins, fibers, and fats. That said, it would be unrealistic to NEVER have processed carbs. Go easy on yourself, take a step back, and assess whether what you eat MOST.
3. Balance is key. Pairing carbohydrate-rich foods with protein, fats, and fibers helps to keep glucose from spiking and falling too quickly. The synergy of pairing foods together will help keep you full and focused between meals as well as support cellular metabolic health.
If you’re still unsure how to adjust your diet and need help, I’m here!
Disclaimer: Please note that “Thyroid School” emails from Chews Food Wisely, LLC (and Nicole Fennell, RD) are not intended to create any physician-patient relationship or supplant any in-person medical consultation or examination. Always seek the advice of a trained health professional about any questions you may have regarding a medical condition and before seeking any treatment. Proper medical attention should always be sought for specific ailments. Never disregard professional medical advice or delay in seeking medical treatment due to information obtained in “Thyroid School” emails. Any information received from these emails is not intended to diagnose, treat, or cure. These emails, websites, and social media accounts are for information purposes only. The information in these emails, websites, and social media accounts is not intended to replace proper medical care.
Works cited:
Bianco AC, Kim BW. Deiodinases: implications of the local control of thyroid hormone action. J Clin Invest. 2006;116(10):2571-2579. doi:10.1172/JCI29812
Peeters RP, Visser TJ. Metabolism of Thyroid Hormone. [Updated 2017 Jan 1]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK285545/
Schweizer U, Köhrle J. Function of thyroid hormone transporters in the central nervous system. Biochim Biophys Acta. 2013 Jul;1830(7):3965-73. doi: 10.1016/j.bbagen.2012.07.015. Epub 2012 Aug 7. PMID: 22890106.
Shahid MA, Ashraf MA, Sharma S. Physiology, Thyroid Hormone. [Updated 2021 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500006/
Refetoff S. Thyroid Hormone Serum Transport Proteins. [Updated 2015 Jun 7]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK285566/
Rousset B, Dupuy C, Miot F, et al. Chapter 2 Thyroid Hormone Synthesis And Secretion. [Updated 2015 Sep 2]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK285550/

EMAIL:
hello@chewsfoodwisely.com
VIRTUAL APPOINTMENTS ONLY
Business Mailing Address:
2525 Robinhood Street
Houston, Texas 77005
© 2026 Chews Food Wisely. All Rights Reserved. Website Designed by AVM
Disclaimers | Privacy Policy | Terms of Purchase | Terms and Conditions