We’ve been told that if we eat enough carrots and sweet potatoes we’ll get enough beta-carotene to meet our Vitamin A needs, but that’s actually not completely accurate. In this post, I will dive into the specifics of the different “types” of vitamin A, the best food sources, how an insufficiency can manifest, whether you should be worried about toxicity, signs of toxicity, and how to pick up signs of Vitamin A deficiency on labs (because it isn’t as straightforward as you might think).
Vitamin A is a powerful fat-soluble vitamin that wears many hats inside the body. The great demand for Vitamin A in the body isn’t always met due to a variety of factors including lack of animal rich foods, increased demands due to inflammation, and other cofactor deficiencies.
We often hear about foods like pumpkin, carrots, and sweet potatoes as being a good source of Vitamin A, which is true in part, but what they’re really rich in is beta-carotene (and other carotenoids). Beta-carotene is a precursor to Vitamin A that humans must convert inactive “active” Vitamin A (retinol) inside the body.
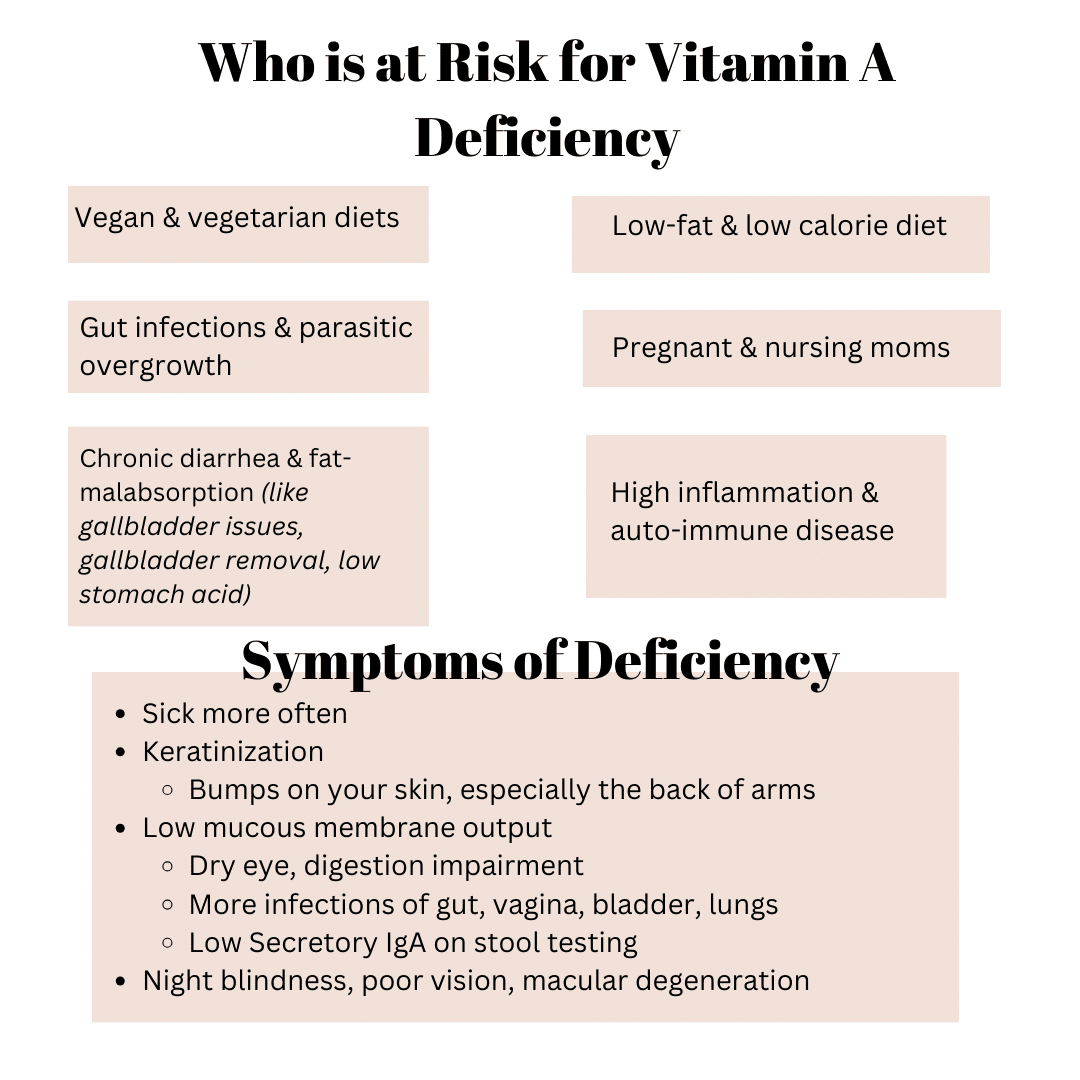
Forms of preformed Vitamin A are found predominantly in animal foods including eggs, liver, organ meats, ghee, salmon, herring, milk and cheese. Therefore, those who follow a vegan or vegetarian diet tend to be at greater risk for Vitamin A deficiency because of their lack of/low intake of preformed Vitamin A rich foods in their diets.
The conversion of beta-carotene happens primarily in the liver and bowels at a rate of 12 mcg beta-carotene to 1 mcg of active Vitamin A. So while beta-carotene is an important antioxidant that helps to combat inflammation, support detoxification, and stabilize the immune response, beta-carotene isn’t adequate enough in typical amounts eaten to provide the amount of Active Vitamin A that the human body needs to function optimally– especially since the average conversion is anywhere from 10-25%.
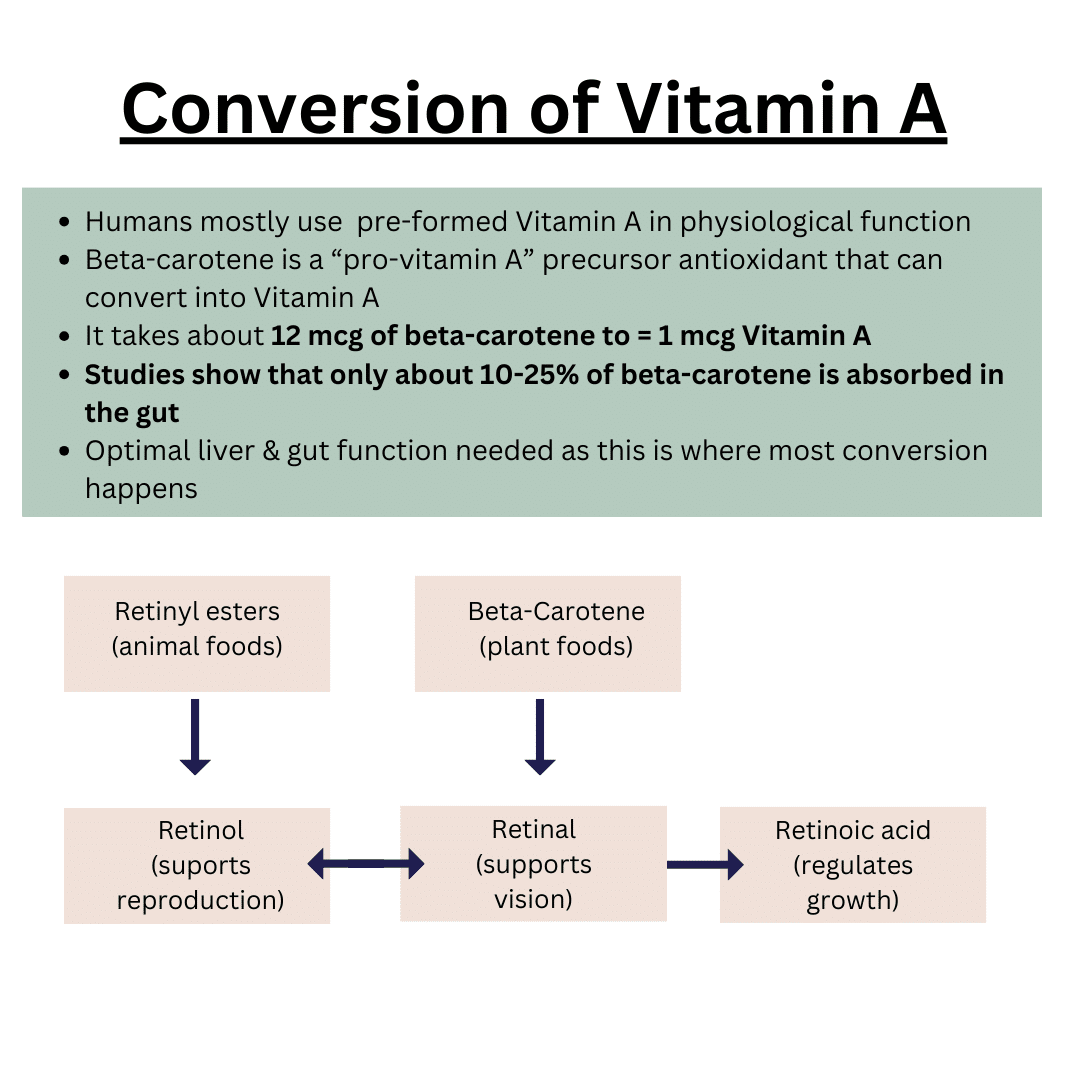
Animal food products provides preformed Vitamin A (aka the form of Vitamin A we most efficiently use):
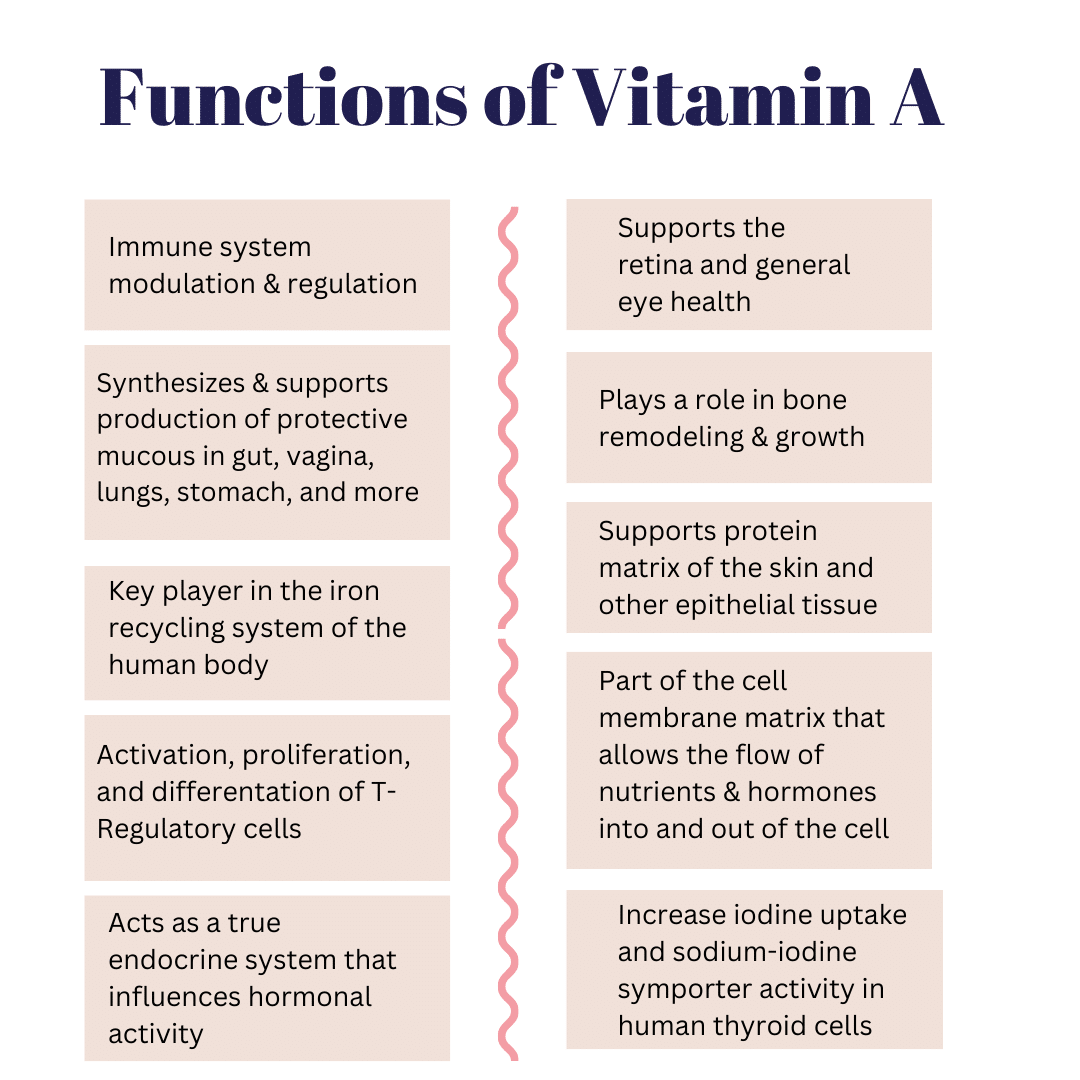
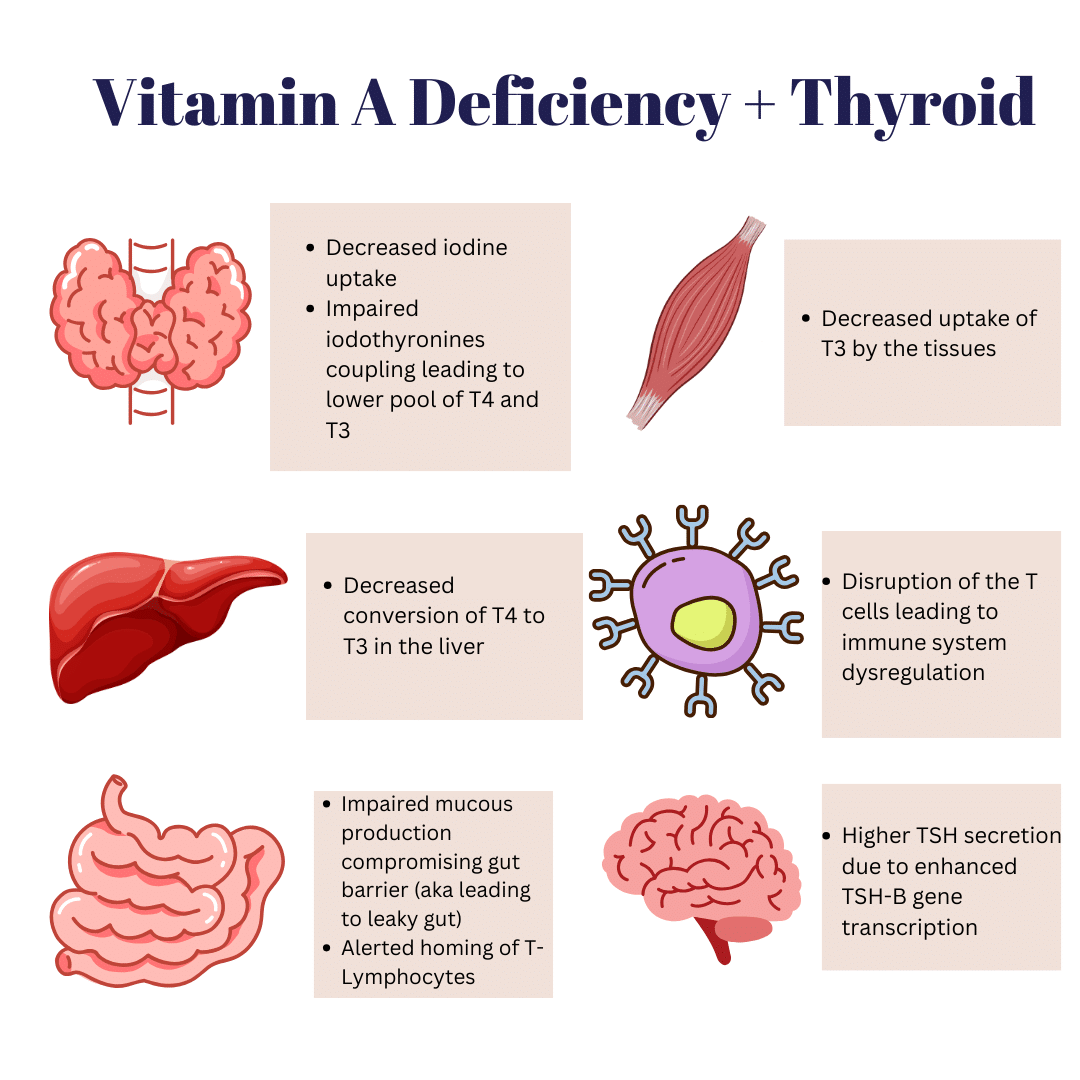
Vitamin A has many jobs in the body ranging from immune system support, to eye health, reproductive support, growth and development, gut health integrity, and yes, even thyroid health! (Keep reading for more specifics on thyroid function & Vitamin A)
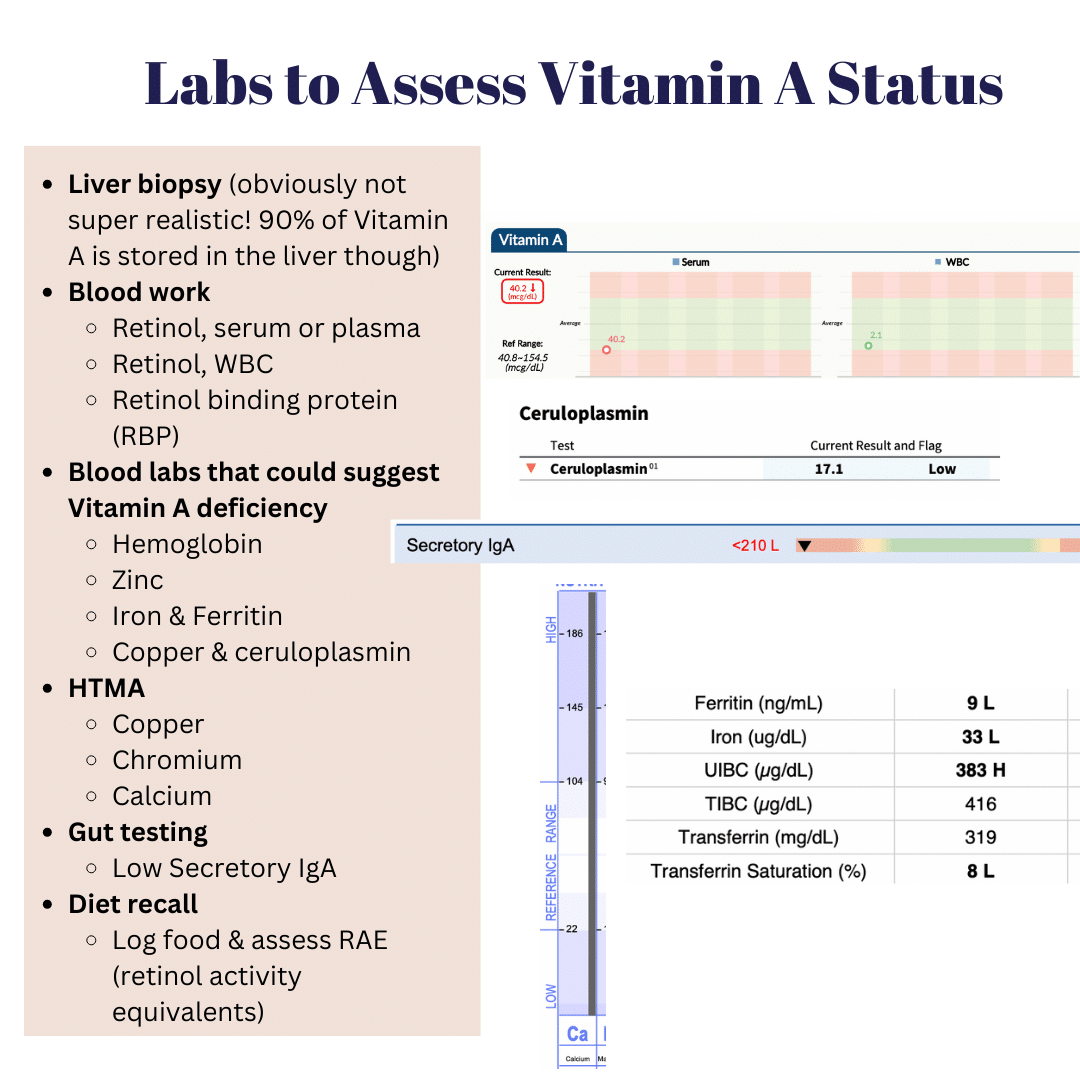
Vitamin A deficiency proper is not as common in developed countries, but Vitamin A insufficiency is rather epidemic. Determining adequate Vitamin A status can be a little tricky sometimes given that 90% of Vitamin A is stored in the liver. However, food recalls and certain blood values can be helpful to provide insight into whether a sub-optimal level of Vitamin A is contributing to many of the symptoms you’re experiencing.
The status of Vitamin A is largely dependent on protein status in the body because Vitamin A is carried and delivered throughout the body on carrier proteins like RBC (retinol binding protein) and transthyretin. This is a big reason why vegan, vegetarians, and those who follow a low calorie and/or low-fat diet are at higher risk of Vitamin A deficiency and insufficiency: lack of protein for carrier proteins, lack of fat for proper Vitamin A absorption, and lack of pre-formed Vitamin A. It can take 1-2 years before symptoms of low levels of Vitamin A show up because Vitamin A is fat-soluble (meaning it gets stored in fat cells). It can show up sooner in children and those who are actively growing (think pregnant women and nursing mothers) because the demand for Vitamin A is higher.
Risk factors:
As with any micronutrient, there is a Goldilocks situation at hand. While too little is problematic, too much Vitamin A, especially since it is fat-soluble (meaning we store a lot in the body) can post risks!
Symptoms of toxicity begin to occur when all binding proteins are saturated. A way to determine this would be to assess Retinol Binding Protein (RBP) on lab work. Toxicity is much more common in those taking high amounts of preformed Vitamin A. More often than not, toxicity from preformed Vitamin A is due to supplement use and not typically from food consumption as food is more self-limiting than supplements. That is, we get FULL from food way before we reach toxic levels. That said, if you go eat an entire polar bear liver in one sitting, you may get acute Vitamin A toxicity. Acute Vitamin A toxicity usually occurs days to weeks after ingestion (studies show ingestion of about 100 times the RDA) and include symptoms such as: headache, blurred vision, nausea, dizziness, aching muscles, and coordination problems.
Many studies have shown that there is not really a toxic level of beta-carotene that you can reach from food alone. However, taken in high amounts from supplements, beta-carotene can actually turn from an antioxidant into a pro-oxidant and promote cell division and destruction of. Vitamin A which can then lead to the Vitamin A deficiency symptoms.
Symptoms of toxicity:

Labeling of Vitamin A on food and supplement packages can be a little confusing because there are a few different ways it can be reported:
One does need to convert into the associated unit in order to determine if the amounts they’re ingesting is safe!
(Recommended Daily Allowance: the amount needed to prevent disease… AKA it is set pretty low)
This RDA is also equivalent to 18,000 IU beta-carotene from food
Adult Male: 3000 mcg or 10,000 IU retinol
Adult Female: 3000 mcg or 10,000 IU retinol
Disclaimer: Please note that “Thyroid School” emails and blogs from and written by Chews Food Wisely, LLC (and Nicole Fennell, RD) are not intended to create any physician-patient relationship or supplant any in-person medical consultation or examination. Always seek the advice of a trained health professional with any questions you may have regarding a medical condition and before seeking any treatment. Proper medical attention should always be sought for specific ailments. Never disregard professional medical advice or delay in seeking medical treatment due to information obtained in “Thyroid School” emails. Any information received from these emails is not intended to diagnose, treat, or cure. These emails, websites, and social media accounts are for information and educational purposes only. The information in these emails, websites, and social media accounts is not intended to replace proper medical care.
References:
https://ods.od.nih.gov/factsheets/VitaminA-Consumer/
https://doi.org/10.1080/07315724.2012.10720431
https://doi.org/10.1093/ajcn/86.4.1040
Carazo A, Macáková K, Matoušová K, Krčmová LK, Protti M, Mladěnka P. Vitamin A Update: Forms, Sources, Kinetics, Detection, Function, Deficiency, Therapeutic Use and Toxicity. Nutrients. 2021 May 18;13(5):1703. doi: 10.3390/nu13051703. PMID: 34069881; PMCID: PMC8157347.
Tang G. Bioconversion of dietary provitamin A carotenoids to vitamin A in humans. Am J Clin Nutr. 2010 May;91(5):1468S-1473S. doi: 10.3945/ajcn.2010.28674G. Epub 2010 Mar 3. PMID: 20200262; PMCID: PMC2854912.
Dwyer J, Saldanha L, Haggans C, Potischman N, Gahche J, Thomas P, Bailen R, Costello R, Betz JM, Andrews K, Gusev P, Pehrsson P, Savarala S, Tey P, Harnly J. Conversions of β-Carotene as Vitamin A in IU to Vitamin A in RAE. J Nutr. 2020 May 1;150(5):1337. doi: 10.1093/jn/nxz334. PMID: 32367133; PMCID: PMC7373782.
Pino-Lagos K, Benson MJ, Noelle RJ. Retinoic acid in the immune system. Ann N Y Acad Sci. 2008 Nov;1143:170-87. doi: 10.1196/annals.1443.017. PMID: 19076350; PMCID: PMC3826166.
Higueret P, Pailler I, Garcin H. Vitamin A deficiency and tri-iodothyronine action at the cellular level in the rat. J Endocrinol. 1989 Apr;121(1):75-9. doi: 10.1677/joe.0.1210075. PMID: 2715762.
Biebinger R, Arnold M, Koss M, Kloeckener-Gruissem B, Langhans W, Hurrell RF, Zimmermann MB. Effect of concurrent vitamin A and iodine deficiencies on the thyroid-pituitary axis in rats. Thyroid. 2006 Oct;16(10):961-5. doi: 10.1089/thy.2006.16.961. PMID: 17042680.
Capriello S, Stramazzo I, Bagaglini MF, Brusca N, Virili C, Centanni M. The relationship between thyroid disorders and vitamin A.: A narrative minireview. Front Endocrinol (Lausanne). 2022 Oct 11;13:968215. doi: 10.3389/fendo.2022.968215. PMID: 36303869; PMCID: PMC9592814.
Smolle J, Wawschinek O, Hayn H, Eber O. Vitamin A und Carotin bei Schilddrüsenkrankheiten [Vitamin A and carotene in thyroid diseases]. Acta Med Austriaca. 1983;10(2-3):71-3. German. PMID: 6880574.
Aktuna D, Buchinger W, Langsteger W, Meister E, Sternad H, Lorenz O, Eber O. Beta-Carotin, Vitamin A und seine Trägerproteine bei Schilddrüsenerkrankungen [Beta-carotene, vitamin A and carrier proteins in thyroid diseases]. Acta Med Austriaca. 1993;20(1-2):17-20. German. PMID: 8475673.
Woźniak D, Drzymała S, Przysławski J, Drzymała-Czyż S. Dietary supplements in hypothyroidism. Acta Sci Pol Technol Aliment. 2021 Oct-Dec;20(4):375-381. doi: 10.17306/J.AFS.0985. PMID: 34724363.
Hinako Homma, Mikio Watanabe, Naoya Inoue, Moeko Isono, Yoh Hidaka, and Yoshinori Iwatani.
Polymorphisms in Vitamin A-Related Genes and Their Functions in Autoimmune Thyroid Disease. Thyroid.Nov 2021.1749-1756.http://doi.org/10.1089/thy.2021.0312
Farasati Far B, Broomand Lomer N, Gharedaghi H, Sahrai H, Mahmoudvand G, Karimi Rouzbahani A. Is beta-carotene consumption associated with thyroid hormone levels? Front Endocrinol (Lausanne). 2023 May 26;14:1089315. doi: 10.3389/fendo.2023.1089315. PMID: 37305054; PMCID: PMC10250628.
Triggiani Vincenzo, Tafaro Emilio, Giagulli Angelo Vito, Sabba Carlo, Resta Francesco, Licchelli Brunella and Guastamacchia Edoardo, Role of Iodine, Selenium and Other Micronutrients in Thyroid Function and Disorders, Endocrine, Metabolic & Immune Disorders – Drug Targets 2009; 9 (3) . https://dx.doi.org/10.2174/187153009789044392
Ihnatowicz P, Drywień M, Wątor P, Wojsiat J. The importance of nutritional factors and dietary management of Hashimoto’s thyroiditis. Ann Agric Environ Med. 2020;27(2):184-193. doi:10.26444/aaem/112331.
Zimmermann MB. Interactions of vitamin A and iodine deficiencies: effects on the pituitary-thyroid axis. Int J Vitam Nutr Res. 2007 May;77(3):236-40. doi: 10.1024/0300-9831.77.3.236. PMID: 18214025.
Rabbani, E., Golgiri, F., Janani, L. et al. Randomized Study of the Effects of Zinc, Vitamin A, and Magnesium Co-supplementation on Thyroid Function, Oxidative Stress, and hs-CRP in Patients with Hypothyroidism. Biol Trace Elem Res 199, 4074–4083 (2021). https://doi.org/10.1007/s12011-020-02548-3
Capriello S, Stramazzo I, Bagaglini MF, Brusca N, Virili C, Centanni M. The relationship between thyroid disorders and vitamin A.: A narrative minireview. Front Endocrinol (Lausanne). 2022 Oct 11;13:968215. doi: 10.3389/fendo.2022.968215. PMID: 36303869; PMCID: PMC9592814.

EMAIL:
hello@chewsfoodwisely.com
VIRTUAL APPOINTMENTS ONLY
Business Mailing Address:
2525 Robinhood Street
Houston, Texas 77005
© 2025 Chews Food Wisely. All Rights Reserved. Website Designed by AVM
Disclaimers | Privacy Policy | Terms of Purchase | Terms and Conditions